
Back اضطراب تعاطي المواد الأفيونية Arabic অ’পিঅইড আসক্তি AS Разстройства, свързани с употребата на опиоиди Bulgarian Addicció als opioides Catalan Trastorno por consumo de opioides Spanish Opioidivieroitusoireyhtymä Finnish התמכרות לאופיואידים HE オピオイド使用障害 Japanese ଓପିଅଏଡ ବ୍ୟବହାର ବେମାରୀ OR Dependência de opioides Portuguese
| Opioid use disorder | |
|---|---|
| Other names | Opioid addiction,[1] problematic opioid use,[1] opioid abuse,[2] opioid dependence[3] |
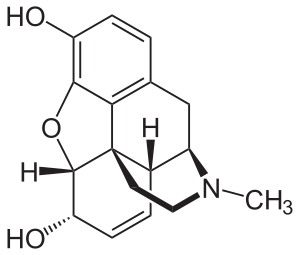 | |
| Molecular structure of morphine | |
| Specialty | Addiction medicine, psychiatry |
| Symptoms | Strong desire to use opioids, increased tolerance to opioids, failure to meet obligations, trouble with reducing use, withdrawal syndrome with discontinuation[4][5] |
| Complications | Opioid overdose, hepatitis C, marriage problems, unemployment, poverty[4][5] |
| Duration | Long term[6] |
| Causes | Opioids[3] |
| Diagnostic method | Based on criteria in the DSM-5[4] |
| Differential diagnosis | Alcoholism |
| Treatment | Opioid replacement therapy, behavioral therapy, twelve-step programs, take home naloxone[7][8][9] |
| Medication | Buprenorphine, methadone, naltrexone[7][10] |
| Frequency | 16 million[11] |
| Deaths | 120,000[11] |
Opioid use disorder (OUD) is a substance use disorder characterized by cravings for opioids, continued use despite physical and/or psychological deterioration, increased tolerance with use, and withdrawal symptoms after discontinuing opioids.[12] Opioid withdrawal symptoms include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood.[5] Addiction and dependence are important components of opioid use disorder.[13]
Risk factors include a history of opioid misuse, current opioid misuse, young age, socioeconomic status, race, untreated psychiatric disorders, and environments that promote misuse (social, family, professional, etc.).[14][15] Complications may include opioid overdose, suicide, HIV/AIDS, hepatitis C, and problems meeting social or professional responsibilities.[5][4] Diagnosis may be based on criteria by the American Psychiatric Association in the DSM-5.[4]
Opioids include substances such as heroin, morphine, fentanyl, codeine, dihydrocodeine, oxycodone, and hydrocodone.[5][6] A useful standard for the relative strength of different opioids is morphine milligram equivalents (MME).[16] It is recommended for clinicians to refer to daily MMEs when prescribing opioids to decrease the risk of misuse and adverse effects.[17]
Long-term opioid use occurs in about 4% of people following their use for trauma or surgery-related pain.[18] In the United States, most heroin users begin by using prescription opioids that may also be bought illegally.[19][20]
People with an opioid use disorder are often treated with opioid replacement therapy using methadone or buprenorphine.[21] Such treatment reduces the risk of death.[21] Additionally, they may benefit from cognitive behavioral therapy, other forms of support from mental health professionals such as individual or group therapy, twelve-step programs, and other peer support programs.[22] The medication naltrexone may also be useful to prevent relapse.[10][8] Naloxone is useful for treating an opioid overdose and giving those at risk naloxone to take home is beneficial.[23] In 2020, the CDC estimated that nearly 3 million people in the U.S. were living with OUD and more than 65,000 people died by opioid overdose, of whom more than 15,000 were heroin overdoses.[24][25]
- ^ a b "FDA approves first buprenorphine implant for treatment of opioid dependence". U.S. Food and Drug Administration (FDA) (Press release). 26 May 2016. Retrieved 16 March 2017.
- ^ "3 Patient Assessment". Clinical Guidelines for the Use of Buprenorphine in the Treatment of Opioid Addiction. Rockville (MD): Substance Abuse and Mental Health Services Administration (US). 2004.
- ^ a b "Commonly Used Terms". www.cdc.gov. 29 August 2017. Retrieved 16 July 2018.
- ^ a b c d e American Psychiatric Association (2013), Diagnostic and Statistical Manual of Mental Disorders (5th ed.), Arlington: American Psychiatric Publishing, pp. 540–546, ISBN 978-0-89042-555-8
- ^ a b c d e Substance Use and Mental Health Services Administration (30 September 2014). "Substance Use Disorders".
- ^ a b "Opioid Use and Opioid Use Disorder in Pregnancy". ACOG. August 2017. Retrieved 16 July 2018.
- ^ a b Cite error: The named reference
BMJ2017Re2was invoked but never defined (see the help page). - ^ a b "Treatment for Substance Use Disorders". Substance Abuse and Mental Health Services Administration. October 2014.
- ^ McDonald R, Strang J (July 2016). "Are take-home naloxone programmes effective? Systematic review utilizing application of the Bradford Hill criteria". Addiction. 111 (7): 1177–87. doi:10.1111/add.13326. PMC 5071734. PMID 27028542.
- ^ a b Sharma B, Bruner A, Barnett G, Fishman M (July 2016). "Opioid Use Disorders". Child and Adolescent Psychiatric Clinics of North America. 25 (3): 473–87. doi:10.1016/j.chc.2016.03.002. PMC 4920977. PMID 27338968.
- ^ a b Dydyk AM, Jain NK, Gupta M (2022), "Opioid Use Disorder", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31985959, NCBI NBK553166, retrieved 16 November 2022
- ^ Diagnostic and statistical manual of mental disorders : DSM-5. Arlington, VA : American Psychiatric Association. 2013. ISBN 978-0-89042-554-1.
- ^ Cite error: The named reference
Brain diseasewas invoked but never defined (see the help page). - ^ Webster LR (November 2017). "Risk Factors for Opioid-Use Disorder and Overdose". Anesthesia and Analgesia. 125 (5): 1741–1748. doi:10.1213/ANE.0000000000002496. PMID 29049118. S2CID 19635834.
- ^ Santoro TN, Santoro JD (2018). "Racial Bias in the US Opioid Epidemic: A Review of the History of Systemic Bias and Implications for Care". Cureus. 10 (12): e3733. doi:10.7759/cureus.3733. PMC 6384031. PMID 30800543.
- ^ Cite error: The named reference
pmid36327391was invoked but never defined (see the help page). - ^ "A Prescriber's Guide to Medicare Prescription Drug (Part D) Opioid Policies" (PDF).
- ^ Mohamadi A, Chan JJ, Lian J, Wright CL, Marin AM, Rodriguez EK, von Keudell A, Nazarian A (August 2018). "Risk Factors and Pooled Rate of Prolonged Opioid Use Following Trauma or Surgery: A Systematic Review and Meta-(Regression) Analysis". The Journal of Bone and Joint Surgery. American Volume. 100 (15): 1332–1340. doi:10.2106/JBJS.17.01239. PMID 30063596. S2CID 51891341.
- ^ "Prescription opioid use is a risk factor for heroin use". National Institute on Drug Abuse. October 2015. Retrieved 16 July 2018.
- ^ Hughes E (2 May 2018). "The Pain Hustlers". New York Times. Retrieved 3 May 2018.
- ^ a b "Trends in the Use of Methadone, Buprenorphine, and Extended-release Naltrexone at Substance Abuse Treatment Facilities: 2003–2015 (Update)". www.samhsa.gov. Retrieved 16 November 2022.
- ^ Donovan DM, Ingalsbe MH, Benbow J, Daley DC (2013). "12-Step Interventions and Mutual Support Programs for Substance Use Disorders: An Overview". Social Work in Public Health. 28 (3–4): 313–332. doi:10.1080/19371918.2013.774663. PMC 3753023. PMID 23731422.
- ^ "Opioid Overdose Prevention Programs Providing Naloxone to Laypersons — United States, 2014". www.cdc.gov. Retrieved 16 November 2022.
- ^ CDC (30 August 2022). "Disease of the Week – Opioid Use Disorder". Centers for Disease Control and Prevention. Retrieved 16 November 2022.
- ^ "Data Brief 294. Drug Overdose Deaths in the United States, 1999–2016" (PDF). CDC. Retrieved 18 May 2018.